EARLY DETECTION
Beyond blood sugar: The hidden link between insulin resistance and type 2 diabetes
13 November 2025

Written by
Ferdinand Skaugerum

Reviewed by

Type 2 diabetes (T2D) often develops for a decade before you are diagnosed. The real problem is not the diagnosis; it is the long, hidden phase of insulin resistance that precedes it.
Many standard health checks test your fasting blood sugar (glucose). This can be an unreliable marker that may appear normal until the damage is already done. For patients with higher risk, doctors also often check long-term sugar levels (HbA1c), which gives more insights.
To truly understand your risk and help prevent the disease, it can help to look deeper: In addition to your long-term sugar levels (HbA1c), also measuring your insulin function, your lipid profile, and the "hidden" visceral fat around and in your organs.
This article explains the difference between the symptoms of type 2 diabetes (e.g., high blood sugar) and its root cause (insulin resistance). We explain what insulin resistance is, how it can develop silently for years, and why a glucose test with normal results might be misleading. We'll also clarify the key markers you could use to get a more detailed picture of your metabolic health.
What is type 2 diabetes?
At its simplest, type 2 diabetes is a chronic condition where your body cannot use insulin effectively. Insulin is a vital hormone. Think of it as the key that unlocks your body's cells to take in glucose (sugar) for energy.
In type 2 diabetes, your cells stop responding properly to insulin. This is called insulin resistance. Your body's response is to produce even more insulin to force the cells to open.
Eventually, your pancreas, which produces insulin, gets exhausted. It can no longer keep up with the high demand. When this happens, sugar cannot get into your cells, so it builds up in your bloodstream, causing high blood sugar. This high blood sugar is the hallmark of type 2 diabetes.
The critical difference: type 1 vs. type 2 diabetes
It is important to know that not all diabetes is the same. The two main types, type 1 and type 2, have very different causes.
Type 1 diabetes is an autoimmune condition
In type 1 diabetes, the body’s own immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. It is genetic, and not caused by lifestyle, and often appears in childhood or young adulthood. A person with type 1 diabetes produces very little or no insulin and must take insulin for the rest of their life.
Type 2 diabetes is a metabolic condition
Type 2 diabetes is the most common form of diabetes, accounting for over 90% of all diabetes cases, and is strongly linked to lifestyle factors and age, which means it can be delayed or prevented.
It is a condition with two main aspects. As described above, it typically begins when your body's cells do not respond normally to insulin, known as insulin resistance. At this stage, your pancreas may be producing normal, or even high, amounts of insulin, but the "key" no longer fits the "lock" on your cells effectively.
Over time, this resistance puts stress on your pancreas. It tries to compensate by working overtime to produce more insulin. Eventually, your pancreas can become exhausted and may lose the ability to produce enough insulin to manage your blood sugar.
So, in type 2 diabetes, you often have a combination of two problems: your cells do not listen to insulin properly, and your pancreas may eventually be unable to produce enough of it.
The first signs are often no signs at all
Some people believe they will feel something when diabetes starts. This is a dangerous misconception.
Why waiting for symptoms can be a failing strategy
The classic symptoms of diabetes are a late-stage warning, not an early one. These symptoms only appear after your blood sugar levels are already consistently high.
They include:
Excessive thirst
Frequent urination
Unexplained fatigue
Blurred vision
Slow-healing sores
If you are experiencing these, your body is probably already in distress. You may have missed the critical window for prevention.
The invisible trigger: Insulin resistance
One of the first signs of type 2 diabetes is insulin resistance (Lee, J., Kim, Mh., Jang, JY. et al., 2023). It is the long, silent prequel to the disease.
For years, even a decade, your body can successfully manage your blood sugar. The problem is how it manages. It does so by pumping out potentially dangerously high levels of insulin. Your blood glucose test may look perfectly fine, but your high insulin can quietly be causing inflammation and damaging your blood vessels.
Is type 2 diabetes a serious health risk?
Yes. It is not a mild condition. Unmanaged high blood sugar is toxic to your body, slowly damaging your nerves and blood vessels.
It is a gateway illness that significantly increases your risk for other serious, life-altering conditions.
The primary complications include:
Heart disease and stroke. This is the number one risk. High blood sugar and high insulin can damage the lining of your arteries, which can lead to blockages.
Kidney disease (nephropathy). Diabetes is a leading cause of kidney failure.
Nerve damage (neuropathy). This can cause pain, tingling, or numbness, especially in your feet and hands.
Eye damage (retinopathy). It can damage the blood vessels in your retina, leading to vision loss and blindness.
Why this matters: The goal of prevention is both to avoid a "diabetes" label, and to prevent the co-morbidities that follow, such as heart attacks, strokes, and kidney failure.
How to get even more insight from your standard health check
Getting a regular check-up with your GP is a good start. Swiss GPs follow evidence- and risk-based national and international guidelines for diabetes screening, and play a vital part in diagnosing and treating diabetes.
Still, unless you are in the target group (e.g., adults 40+ or have other risk factors), you may not get as extensive tests, such as long-term blood sugar (HbA1c) or insulin resistance (HOMA Index). And a regular check-up may not include a body composition or measure of visceral fat.
The normal blood sugar trap
A standard Swiss health check (Vorsorgeuntersuchung) is a strong foundation for preventive care, especially for detecting many common health issues. However, fasting glucose alone cannot always capture early metabolic changes. For those wanting a more complete picture, additional tests – like fasting insulin or MRI-based fat mapping – can provide valuable extra insights.
Your body is a master of compensation. It will work overtime for years to keep that single glucose number in the normal range. This may give the impression of normality even when early metabolic changes are present. The fasting glucose measure might indicate that everything is good, while under the surface, your body is fighting a losing battle with insulin resistance.
The gap in the data: Where is your fasting insulin?
A doctor will often add an HbA1c test (your 3-month average blood sugar) if you are already seen as at-risk – for example, if you have a family history or are overweight.
Fasting blood sugar and HbA1c levels can give a good view of your blood sugar levels. But for a healthy, asymptomatic individual, a critical marker is still missing from routine screens: fasting insulin.
Measuring fasting insulin can complement your fasting glucose and HbA1c results, helping to reveal how efficiently your body manages blood sugar behind the scenes; it can shed light on how hard your body is working to manage your blood sugar. In that way, high insulin can be an early warning sign for type 2 diabetes. These may not be part of routine screening because they are used selectively based on individual risk.
Why this matters: A glucose test with normal results can mean that you are genuinely healthy. It could also mean that you are in the final stages of pre-diabetes, just before your pancreas gives out. Adding insights from insulin resistance helps turn a good check-up into a truly comprehensive picture of your metabolic health.
A modern approach: The markers that actually matter
To truly understand your metabolic health and catch pre-diabetes, you must look deeper than a fasting blood sugar test.
Marker 1: HbA1c (Hemoglobin A1c)
This test measures your average blood sugar level over the past 2-3 months. It is not a snapshot like a fasting glucose test. It tells the true story of your body's average glucose environment and is a far more stable, reliable marker than fasting blood sugar alone.
Marker 2: Fasting insulin and HOMA-IR
This is an important test for early prevention of type 2 diabetes, yet it is rarely performed in a standard check-up. High fasting insulin is the first sign that your cells are becoming resistant.
Your fasting insulin and glucose levels are used to calculate your HOMA-IR score. This is a direct estimate of your insulin sensitivity and an important, early indicator of pre-diabetes (Lee, J., Kim, Mh., Jang, JY. et al., 2023).
Marker 3: Your lipid profile (ApoB and Triglycerides)
Diabetes is a metabolic disease. A classic sign of insulin resistance is a dysfunctional lipid profile, specifically high triglycerides and a high ApoB level. ApoB measures the count of all "bad" cholesterol particles (e.g., low-density lipoprotein), which is a more accurate predictor of heart disease risk than standard cholesterol tests.
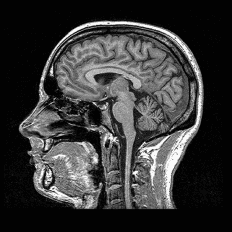
The hidden risk factor: What a full-body MRI reveals
Your metabolic risk is not just in your blood. It is also influenced by where your body stores fat.
Visceral fat: The dangerous fat you cannot see
You have two main types of fat. Subcutaneous fat is the "pinchable" fat under your skin. Visceral fat is the "hidden" fat deep in your abdomen, partially infiltrating and wrapped around your organs like your liver, pancreas, and intestines.
Visceral fat is metabolically active and toxic. It releases inflammatory substances that directly interfere with your organs' functions, dramatically driving insulin resistance. You can be thin on the outside but have high levels of this dangerous internal fat. A full-body MRI is the most precise way to quantify your visceral fat volume.
Non-alcoholic fatty liver disease (NAFLD)
When your liver becomes infiltrated with fat (a condition an MRI can clearly detect), it stops responding properly to insulin. This forces your pancreas to work even harder and accelerates your path toward type 2 diabetes.
What happens when you are diagnosed?
If you are diagnosed with pre-diabetes or early type 2 diabetes, it may not be a life sentence. But it is a critical call to action.
Can type 2 diabetes be cured?
In line with medical guidelines, there is no cure for type 2 diabetes. However, it can often be put into remission.
Remission means you have returned your blood sugar levels to a normal range without needing medication. You achieve this through significant, sustained lifestyle changes. It is a powerful testament to the body's ability to heal.
The most important prevention: Management and lifestyle
Prevention and remission are built on the same foundation. It is about making sustainable changes, rather than adopting an extreme, restrictive diet.
What to reduce: The biggest impact comes from reducing ultra-processed foods, sugary drinks, and refined carbohydrates (like white bread, pastries, and pasta) that spike your blood sugar and insulin.
What to increase: Focus on protein, healthy fats, and fiber (especially from vegetables). These foods help stabilize your blood sugar, keep you full, and reduce the burden on your pancreas.
The other keys: Regular movement is essential. Strength training is particularly effective, as building muscle gives your body a place to store glucose, pulling it out of your bloodstream. Prioritising sleep is also critical, as poor sleep immediately worsens insulin resistance.
Your action plan: Move from reactive to preventive
You should not have to wait for symptoms to take control of your health. If you are a health-conscious person who wants a clear baseline, you probably want (and need) data.
Stop guessing. Start measuring.
Instead of wondering if you are at risk, you can get a precise, data-driven answer.
At Ahead, we offer an Advanced blood test designed for exactly this. It includes all the important blood markers to detect type 2 diabetes mentioned above (like HbA1c, fasting insulin, and ApoB).
Our AI-based body composition (included in our Advanced and Pro packages) uses advanced full-body MRI imaging to measure fat and muscle distribution and understand their effect on your metabolism, strength, and lasting health.
The Advanced blood test is a good place to start. Combining it with the body composition analysis can give you a more complete, 360-degree view of your metabolic health – from your average long-term blood sugar to the potentially dangerous visceral fat around your organs.